Since 2008, Stratis Health has pioneered processes for establishing and supporting palliative care services in smaller, rural communities. Recognizing that existing best practices were designed for large hospitals, Stratis Health has addressed this gap by working with more than 40 rural communities across the country to build capacity to offer palliative care services.
To increase access to palliative care services in rural areas, Stratis Health leads efforts to assist communities in developing programs and building skills to improve advance care planning, symptom management, communication, coordination, and delivery of care to improve the quality of life and care for those with chronic diseases or life-limiting illness.
Using a strength-based approach, community-based teams identify their goals and resources and then develop plans for implementation focusing on current assets and resources. A variety of tools and resources are available to support this approach:
Rural Community-based Palliative Care Framework
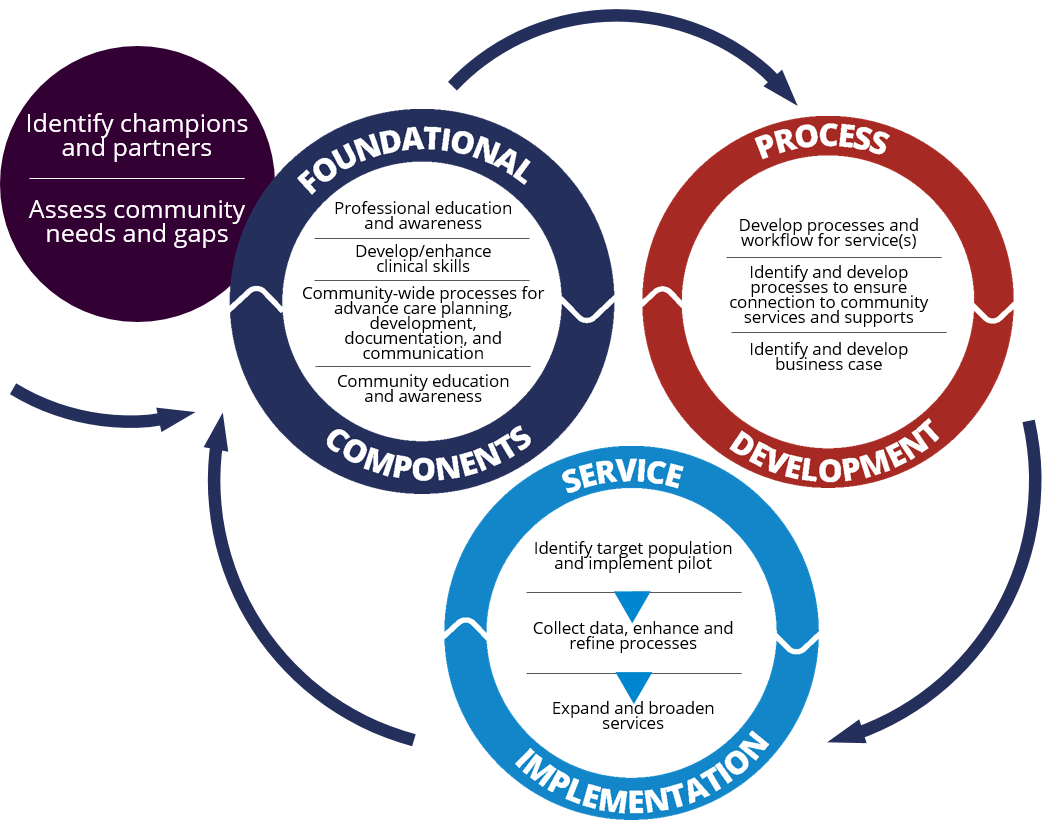
Stratis Health developed a framework for rural community-based palliative care program development reflecting foundational components, process development, and service implementation including a toolkit that contains guidance and links to a comprehensive set of resources to support rural leaders in developing community-based palliative care services.